Tackling the deadliest cancer type
Our lung cancer research
This month is Lung Cancer Awareness Month. Lung cancer is the third most common cancer in the UK, with 46,700 new cases diagnosed each year. Approximately 35,600 people lose their lives annually as a result of lung cancer in the UK, making it the most common cause of cancer-related mortality. Only 5% of those affected survive their cancer for 10 years or more in the UK, and this survival rate has not shown much improvement over the last four decades. For this reason, lung cancer is classified as a Cancer Research UK (CRUK) cancer of substantial unmet need, and is one of the main cancer types on which research is focused here at the Barts CRUK Centre.
Our lung cancer research is generously supported by a variety of charities and funding bodies, including Barts Charity, BBSRC, British Lung Foundation, CRUK and the Medical Research Council.
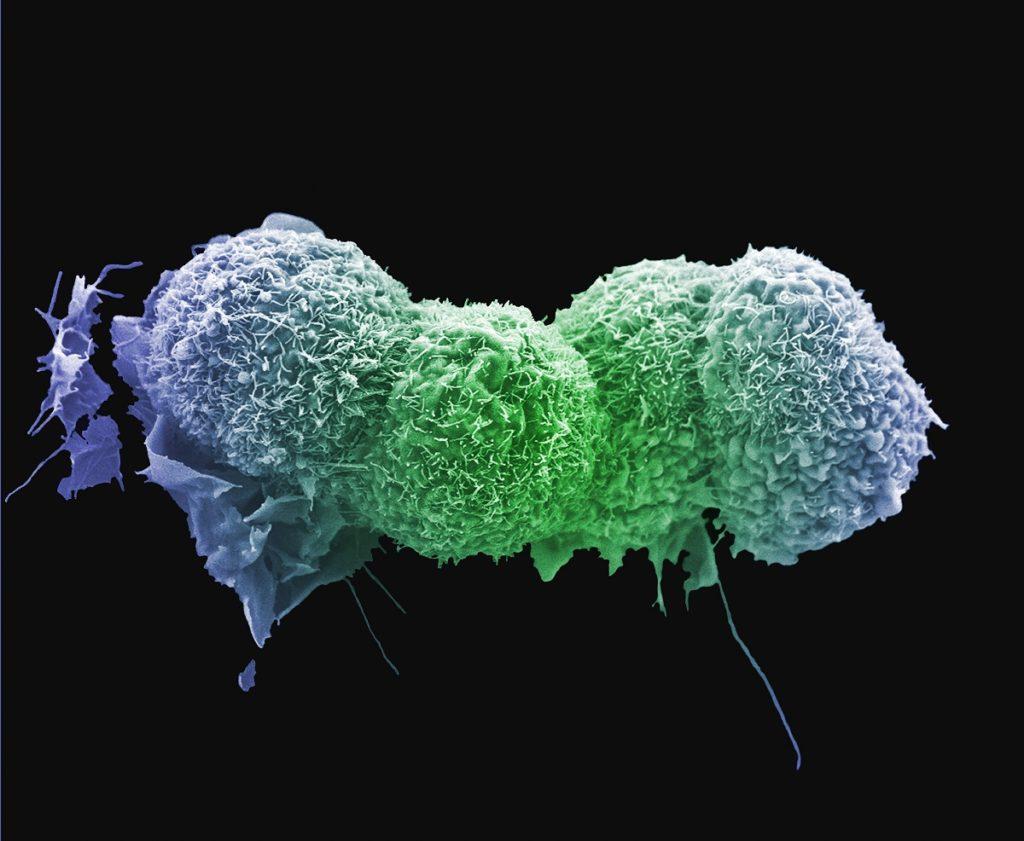
Understanding the basic biology
Our research spans from laboratory experiments to better understand the basic biology of lung cancer, to direct translation into clinical trials. In order to find new treatments that can improve the lives of cancer patients, it is essential to understand the changes that occur in normal cells that drive cancer development.
A recent study led by Professor Tyson Sharp, Lead for our Centre for Molecular Oncology, identified a novel mechanism implicated in the development of lung adenocarcinoma (the most common type of non-small cell lung cancer), mediated by the loss of a gene called LIMD1. Analyses revealed that LIMD1 is lost in almost half of lung adenocarcinoma cases, and the team now endeavour to develop a therapy to target LIMD1 loss in lung cancer. It is hoped that targeting this defect will prove to be an effective treatment option.
From bench to bedside
 A new clinical trial led by Professor Peter Szlosarek, called iTRAP, is due to launch next year and will evaluate the use of a new drug combination for patients with advanced non-squamous non-small cell lung carcinoma (NSCLC). The treatment regimen will combine chemotherapies ADI-PEG20, pemetrexed and carboplatin with immunotherapy atezolizumab.
A new clinical trial led by Professor Peter Szlosarek, called iTRAP, is due to launch next year and will evaluate the use of a new drug combination for patients with advanced non-squamous non-small cell lung carcinoma (NSCLC). The treatment regimen will combine chemotherapies ADI-PEG20, pemetrexed and carboplatin with immunotherapy atezolizumab.
This drug combination will be tested in patients whose tumours lack the ASS1 protein, which makes them sensitive to the drug ADI-PEG20. The ASS1 protein is responsible for the production of a key amino acid, called arginine, required for the growth and metabolism of aggressive tumours. When tumours lack the ASS1 protein and cannot produce their own arginine, they rely on the arginine in the blood supply to fuel their growth. ADI-PEG20 works by depleting arginine in the blood, thus starving the tumours of this essential amino acid.
ADI-PEG20 has shown promising results in previous clinical trials when combined with other chemotherapies. Investigators will now look at whether the ADI-PEG20, pemetrexed and carboplatin chemotherapy combination can be improved by the addition of atezolizumab, an immune checkpoint inhibitor, in the first clinical trial in the world to test this quadruplet drug combination.
Chemoimmunotherapy has been shown to be more effective than either chemotherapy or immunotherapy alone and the investigators hope that this new drug combination will offer an effective treatment option for patients with NSCLC.
We are committed to ensuring that discoveries in the laboratory feed through our translational pipeline to improve cancer prevention, diagnosis and treatment. Our researchers will continue to work to better understand the early events that initiate lung cancer development, with the aim of identifying innovative therapies to help those affected by this devastating disease.
- Thank you to our funders for your continued support of our lung cancer research -
Category: General News

No comments yet