The REMODEL project: Remodelling tumour microenvironments to improve immunotherapy
Professor Fran Balkwill from Barts Cancer Institute at Queen Mary University of London has received a UK Research and Innovation (UKRI) Frontier Research grant of over £2 million to investigate the most effective ways to remodel cancers to enhance the effects of immunotherapy.
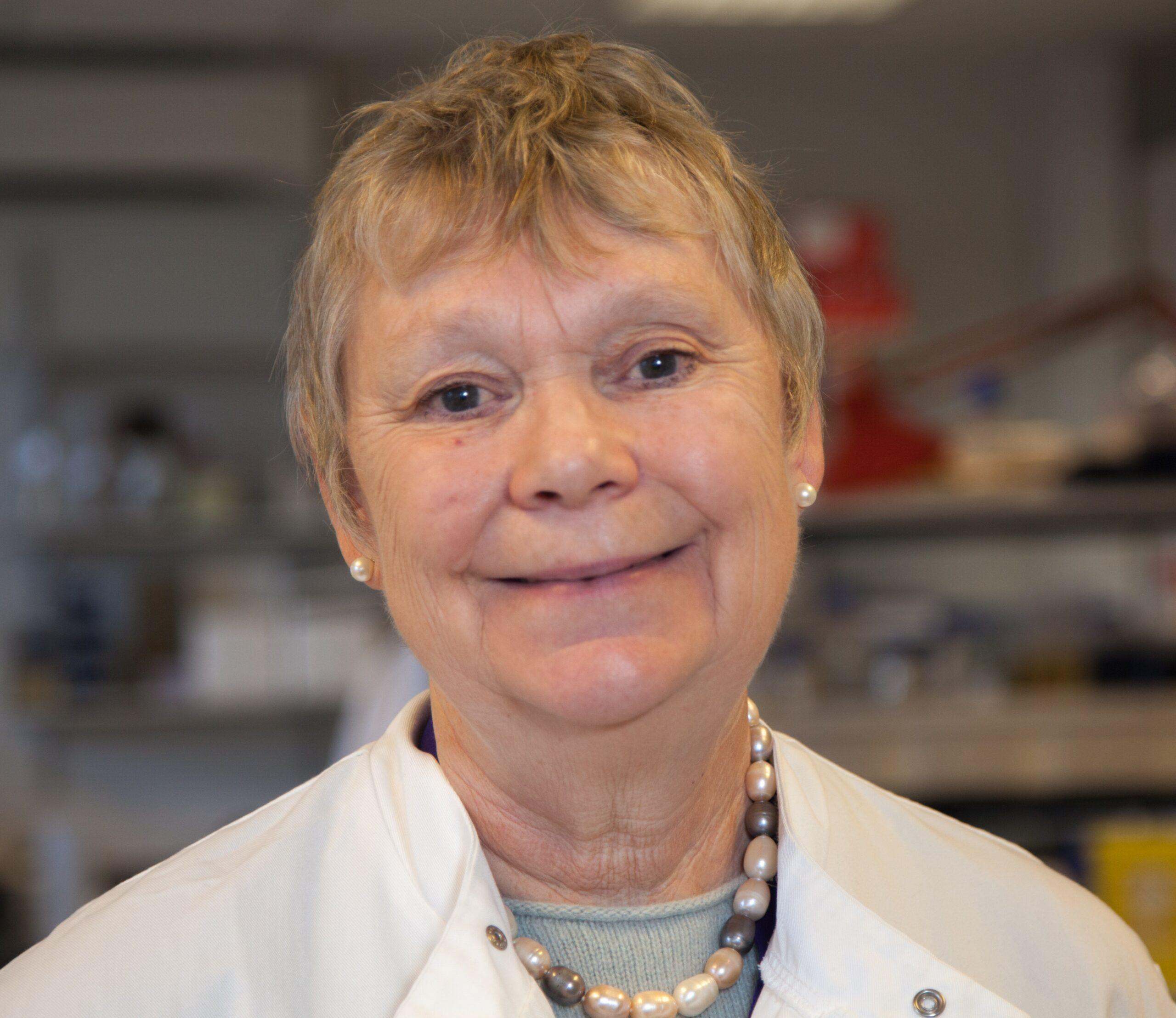
Professor Balkwill and her team have developed 3D multi-cellular models of the human ovarian tumour microenvironment (TME) in the laboratory. In the REMODEL project, the team will now use these models to understand how immune cells within the TME kill cancerous cells and, based on their findings, how the TME can be remodelled to enhance immune cell killing capacity.
Professor Balkwill said:
“Immunotherapies harness the power of the body’s immune system to fight cancer, however only a minority of patients currently benefit from this type of treatment. I hope that this project of remodelling cancer microenvironments to improve immune cell killing of cancerous cells can help to change this to a majority.”
Cancer cells do not exist in isolation within tumours; they interact with (and often corrupt) other healthy cells, such as immune cells and structural cells, as well as structural molecules. The cancer cells, healthy cells and molecules constitute the TME, and their interactions support the growth, evolution and spread of the tumour.
Understanding the interactions between cancer cells and the rest of the TME, as well as having the models to interrogate these interactions, is essential to devise new therapeutic strategies against cancer.
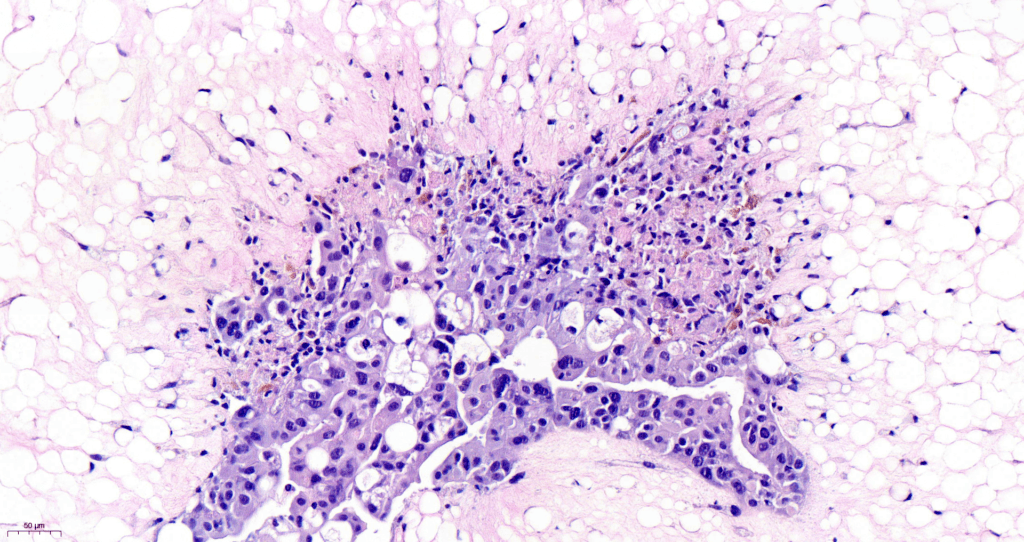
Over the last decade, Professor Balkwill and her team have been working to build mini-models of the human TME in the laboratory. To do this, the team first deconstructed human samples of a common site of cancer spread in ovarian cancer called the omentum, to characterise the different cell types (and their proportions) present in the TME.
This deconstruction provided the building blocks needed to re-construct 3D multi-cellular cancer models in the laboratory using cells obtained from cancer biopsies. The novel models recapitulate the complex interactions between cancer cells and their microenvironment.
Identifying barriers to immunotherapy
In the REMODEL project, the team will harness the 3D cancer models to understand the interactions between cancer cells and the TME, and how these interactions can be modified to improve the success of immunotherapy.
Immunotherapies work by giving the body’s own immune cells a boost to help them identify and kill cancer cells. Examples of immunotherapies include CAR T cells and gamma delta lymphocytes, which are immune cells that have been isolated from a patient’s blood and engineered in the laboratory to recognise cancer cells before they are injected back into the patient as treatment.
Although immunotherapies have shown promise in a variety of cancer types, particularly blood cancers, they have had limited success in solid tumours such as ovarian cancer.
For immunotherapy to be successful, immune cells have to be able to access the cancer cells within the tumour, but the TME can act as a physical and chemical barrier to keep immune cells out. In addition, the structural molecules that support the tumour (known as the extracellular matrix or ECM) can stop immune cells from recognising cancer cells.
The team will generate models with different characteristics using four different cell lines of high-grade serous ovarian cancer (HGSOC), the most common type of ovarian cancer in Europe, and malignant cells from ovarian cancer biopsies. They will add TME components to the models including adipocytes (fat cells), fibroblasts (cells involved in making the ECM) and mesothelial cells (cells that form a protective barrier on tissues) from human omentum obtained from patients during cancer surgery.
Using these models, the team will be able to study and generate novel data on how the different types of cancer cells interact with other components of the TME.
To study immune cell interactions in their models, the team will embed the mini tumours into a plastic chip that mimics the conditions of the TME, including blood flow. Through blood vessels that they grow in the chip, the team will deliver CAR T cell and gamma delta lymphocyte immunotherapies into the tumours and identify the barriers immune cells encounter that prevent them from killing the cancer cells.
Remodelling the TME to enhance immune cell killing
The models will provide a valuable pre-clinical platform for testing treatments to improve the success rates of immunotherapies.
The team will identify drug inhibitors that target and remodel key components of the TME and assess their effectiveness at removing the barriers impeding immune cell killing capacity. By adding the drug inhibitors to the 3D models followed by the addition of the immunotherapies, the team will measure how well immune cells can access and kill the cancer cells in the models in response to the treatment combination.
Professor Balkwill added:
“REMODEL tackles an important challenge - understanding and modelling the human TME for therapeutic benefit. This project will take complex 3D human cell models to new levels, and provide ways to accelerate and improve pre-clinical testing of immune- and other cancer therapies, as well as refining and reducing the use of animal models.”
More information:
- REMODEL is funded under the UKRI EPSRC Frontier Research Guarantee as a UKRI Frontier Research grant [number EP/X028704/1]
- News item: Building a human tumour microenvironment in the lab – updates from the CanBuild Project
Category: General News, Grants & Awards

No comments yet