Biological clues in tissue surrounding breast tumours could indicate likelihood of cancer recurrence
A new study led by Barts Cancer Institute (BCI), Queen Mary University of London, has identified molecular characteristics in ‘normal-looking’ tissues surrounding breast tumours that may indicate whether breast cancer is likely to return following surgical removal of the tumour. Such biological clues could help to identify patients at risk of recurrence and help to guide treatment decisions.
Breast screening programmes and improved self-monitoring have led to significant improvements in the early detection of breast cancer. If breast cancer is detected at an early stage, breast-conserving treatment may be an option – this involves the surgeon removing the area of cancer and a border of surrounding breast tissue. Despite successful removal of the tumour with seemingly cancer-free borders (determined by examination under the microscope), up to 40% of women may develop recurrence of their breast cancer following breast-conserving treatment.
Previous research suggests that missed residual microscopic disease or genetic alterations in the normal tissue left behind after surgery may contribute to an increased risk of cancer recurrence. With this in mind, the present study, funded by Barts Charity, set out to learn more about the molecular alterations in ‘normal-looking’ tissues surrounding primary breast tumours, and to determine whether these alterations provide an indication of the likelihood of cancer recurrence in patients.
Novel insights into ‘normal’ breast tissue
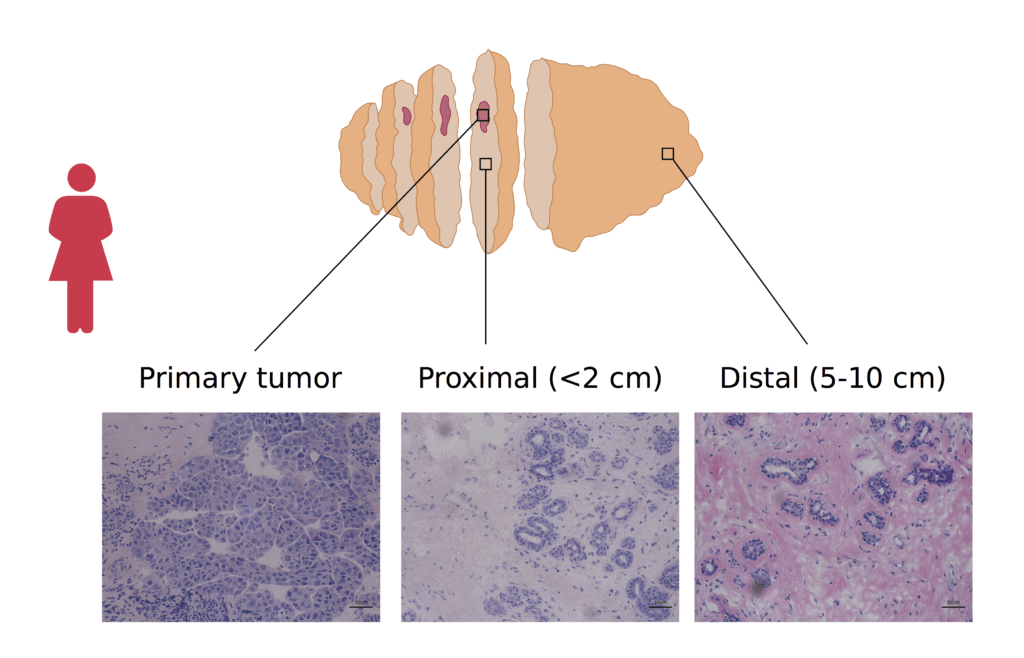
Led by BCI Professors Louise Jones and Claude Chelala, the team conducted in-depth analyses of breast cancer samples and morphologically normal tissue close to the tumour (<2 cm away) and distant from the tumour (5-10 cm away). Unlike previous studies that have reported genetic errors at surgical borders 4 cm away from the tumour, the team identified alterations in tissues located as far as 10 cm from the primary tumour. However, it was the molecular characteristics of the tissues that had the greatest predictive value of cancer recurrence, rather than their distance from the tumour.
By analysing the morphologically normal breast tissue samples, the team were able to identify four subtypes of tissue, each with distinct molecular features. One subtype, named the metabolic subtype, was associated with a significantly poorer outcome for the patient compared with the other subtypes.
The findings were published in npj Breast Cancer (https://www.nature.com/articles/s41523-020-00182-9).
First author of the study, Dr Emanuela Gadaleta said:
"This is an exciting field of research that offers the opportunity to tease out novel insights into so-called normal tissues and understand their involvement in breast cancer. With the data generated by this study being returned to the Breast Cancer Now Tissue Bank and being made available to researchers, I hope that future projects will be able expand on our research and truly realise the aspiration of personalised medicine."
PhD student Pauline Fourgoux, second author of the study, added:
“Characterising these changes in morphologically normal breast tissue is vital. Margin excision could be monitored differently in the future which would impact the number of patients having cancer recurrence after a breast-conserving treatment.”
Unlocking the prognostic potential of ‘normal’ breast tissue
Professor Chelala said:
“With the generous support from Barts Charity, we used various types of data generated on carefully annotated samples from the Breast Cancer Now Tissue Bank (BCNTB). By bringing these data together, we had the unique opportunity to transform otherwise disparate clinical, molecular and pathological data into real value for breast cancer care. With the support of BCNTB, our data will be returned to the Bioinformatics portal of the BCNTB where researchers could query our findings and request matched specimens for further studies.”
Although breast cancer survival in the UK has doubled in the last 40 years, it remains the 4th most common cause of cancer mortality.1 This study has made the first steps towards unlocking the prognostic potential of normal tissue in the affected breast of breast cancer patients. The findings suggest that the surrounding breast tissue should be analysed in addition to the tumour, with insights gained from such analyses helping to identify patients who would benefit from specific therapeutic interventions.
Professor Jones added:
“This study emphasises the huge importance of access to high quality tissue samples to really help understand disease, and we are immensely grateful to our patients who donated samples and made this possible. The key finding of predictive molecular signatures in non-tumour tissue opens up opportunities to stratify patient care and surveillance. It’s wonderful that Barts Charity were able to support this work.”
The research was performed in collaboration with researchers from Queen Mary’s Life Science Initiative Centre for Computational Biology and School of Biological and Chemical Sciences.
1Cancer Research UK, Breast Cancer Statistics. Accessed August 2020.
https://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/breast-cancer
Category: General News, Publications

No comments yet