Unexpected inhibitor of breast cancer invasion revealed
Scientists have uncovered a molecule with a surprising ability to inhibit early breast cancer cells from invading surrounding tissues according to a new publication from Barts Cancer Institute (BCI), Queen Mary University of London. The findings shed light on the complex factors that drive early-stage breast cancer progression and could also help us to identify ways to distinguish people who need treatment from those for whom treatment could cause needless harm – so-called ‘overtreatment’.
Leading the study was Dr Shayin Gibson, who recently completed her PhD and published the new paper under the guidance of co-senior author Professor Richard Grose. The study was also led by co-senior author Dr Ed Carter, a former postdoctoral researcher in Professor Grose's team who now leads his own group at the University of Bath. We spoke to Dr Gibson about the implications of the new findings and her journey to reach them.
A balancing act: to treat or not to treat
Breast cancer is the most common cancer in the UK, with around 55,900 cases every year – more than 150 every day. Thanks to advances due to research, UK breast cancer survival has doubled in the past 50 years. But there’s still much more to be done: the condition remains the second most common cause of cancer death in women, with around 11,400 deaths every year.
Dr Shayin Gibson has spent the past four years of her PhD in Professor Richard Grose’s lab at the BCI, researching ductal carcinoma in situ (DCIS), a form of breast cancer that has not invaded into the surrounding breast tissue. Her aim was to identify factors that contribute to the progression of DCIS to invasive breast cancer.
Around 30–50% of people with DCIS will go on to develop into invasive breast cancer that spreads to other tissues. But in many cases, DCIS cases can remain stable and won’t threaten their health. So how can we tell who urgently needs treatment – such as surgery to remove part or all of a breast – and who can be spared unnecessary treatment?
“The incidence of DCIS has increased recently,” Dr Gibson explains, “but the question is: are there actually more cases or have we just become better at detecting it? There’s a lot of discussion in the field around how we can avoid overtreating patients, especially those whose DCIS may not cause them any harm during their lifetime.”
"There’s a lot of discussion in the field around how we can avoid overtreating patients, especially those whose DCIS may not cause them any harm during their lifetime.”
— Dr Shayin Gibson
Dr Gibson has been studying the complex neighbourhood of cells and molecules that surrounds cancerous cells in DCIS – known as the microenvironment – which heavily influences the condition’s development. She has been searching for clues as to what drives cancer to become invasive in some people, and what helps control the cancer and prevent it from progressing in others.
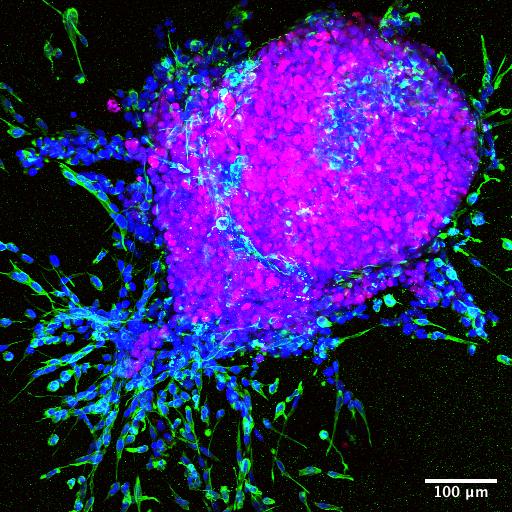
She’s particularly interested in molecules called proteases – microscopic scissors that cut up proteins. Typically, scientists see these molecules as helping to promote tumour growth by cutting up a structure called the extracellular matrix – a scaffolding system that surrounds our cells and helps create the 3D structure of the tissue. Cutting up this matrix can create an escape route that cancer cells migrate through, enabling them to break free and spread to other tissues.
But surprisingly, Dr Gibson and the team in Professor Grose’s lab discovered that a protease called ADAMTS3 seems to do the exact opposite: it suppresses the invasive spread of DCIS. The findings, published in Matrix Biology, represent a highlight of Dr Gibson’s PhD journey.
Interestingly, the team found that levels of ADAMTS3 in the microenvironment were lower in invasive breast tumours compared with healthy breast tissue, suggesting that ADAMTS3 might have tumour-suppressing effects. What’s more, when the researchers reduced the amount of ADAMTS3 in a lab model that mimics DCIS progression, the cells became more invasive. Could the amount of ADAMTS3 help us to predict how likely a person’s DCIS is to become invasive?
International teamwork
This discovery grew out of an international collaboration. Dr Gibson travelled to Copenhagen, where she spent five weeks with a team at the Technical University of Denmark mastering a novel technique called TAILS that would be central to her findings.
“Having the opportunity to go to Copenhagen was really valuable,” Dr Gibson comments. “Richard supported me to take on that challenge and represent him and the institute – I learned a lot from that.”
Using the TAILS technique, Dr Gibson discovered that ADAMTS3 cleaves a molecule in the extracellular matrix called fibronectin that would otherwise support tumour growth and invasion. She unpicked a number of complex interactions at play, finding that fibronectin stimulates tumour invasion by binding to a molecule on the surface of cells called integrin α5β1. These new insights shed important new light on how these different molecules can promote or inhibit breast cancer development in the early stages of the disease.
The findings suggest that looking at the amounts of these different molecules – ADAMTS3, fibronectin or integrin α5β1 – in people with DCIS could present a promising new way to predict how likely their cancer is to become invasive and require treatment. However, further work is needed to confirm these findings, including more detailed studies of patient tumours that later become invasive.
By better understanding the myriad of factors that can provoke or prevent early-stage breast cancer from developing into invasive disease, we can begin to build more accurate predictions of how each patient’s unique condition will progress. This will lead us towards a more personalised approach to tackling the disease, enabling doctors to select the best treatment plan to support a long and healthy future for each individual.
Life as a PhD student at Barts Cancer Institute
Reflecting on her scientific journey, Dr Gibson looks back on the formative impact that the BCI has had on her career. She recalls, "During my undergraduate degree, I did a placement year at the BCI in Professor Peter Schmid's lab, looking at drug resistance in breast cancer. It was my first time working in a laboratory, and it was that experience of working alongside PhD students, postdocs, and world-leading principal investigators that really sparked my ambition to come back and undertake a PhD at BCI.”
“During my PhD, I’ve felt really supported by Richard and by the Institute. It can be easy to feel isolated during a PhD, but I haven’t felt that because of the culture here. There’s so much collaboration within the different centres and there’s a great social aspect too, which I’ve really valued.”
Professor Grose commented: “Shayin has been a fabulous PhD student and it is wonderful to see her graduate with two first author research articles that have revealed exciting insights into the importance of the proteolytic landscape in early breast cancer. We are going to really miss her in the Centre for Tumour Biology, but look forward to watching her continued success!”

This study was funded thanks to Cancer Research UK, Breast Cancer Now, Barts Charity and the Rosetrees Trust.
Category: General News, Publications

Ian Hart 11/08/2023
Well done Dr Gibson! This work could have very important ramifications and I look forward to reading about your future studies.